Abstract
Introduction
Direct Antiglobulin Test (DAT) positivity occurs at higher rates in patients with Non-Hodgkin Lymphoma and is often associated with poor prognosis. This study examined the genetic differences between DAT positive (DAT +) and DAT negative (DAT-) DLBCL cases, and the effect of DAT positivity on survival and revised international prognostic index (R-IPI) in Diffuse Large B-Cell Lymphoma (DLBCL).
Method
One hundred and thirteen cases that had undergone DAT testing at the time of diagnosis as part of a lymphoma screen were included. DAT was performed by the column agglutination method. Cell of origin was determined using the Hans criteria. DNA was extracted from 7 DAT+ and 8 DAT- patient samples and targeted next-generation sequencing (NGS) was performed. Non-synonymous mutations were then grouped into B-cell pathways in DAT+ and DAT- groups. Analysis of survival outcomes was assessed by the Kaplan-Meier method and Cox proportional hazards regression.
Results
The median age of the cohort was 65.0 (Interquartile Range [IQR] 55.3-74.5) and the median follow up time was 2.1 years (IQR 0.7-5.0). Of the 113 cases, 23 (20.3%) were positive and 90 cases (79.7%) were negative. One of the DAT+ cases was diagnosed with clinical autoimmune hemolytic anaemia at the time of DLBCL diagnosis. The DAT+ group were significantly more likely to have a lactate dehydrogenase (LDH) level > upper limit of normal (ULN) at the time of diagnosis (91.3% vs 67.4%, p=0.034), and to be of non-Germinal Centre (non-GC) origin (63.2% vs 33.3%, p=0.033).
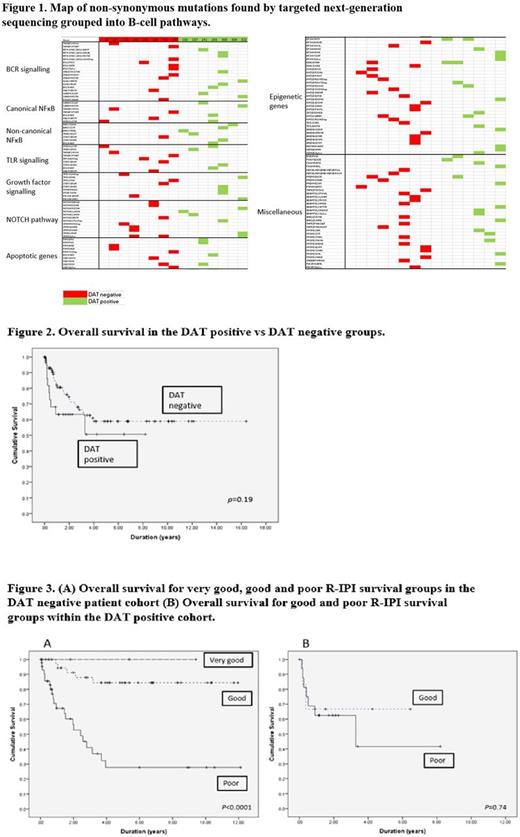
An average of 10.07 mutations per DLBCL clone were found on NGS (DAT+ 10.14 vs DAT-10.00). Mutations were found in genes and B-cell pathways associated with oncogenesis and autoimmunity in both the DAT+ and DAT- groups. The most recurrently mutated genes were KMT2D (n=13), MYOM2 (n=9), EP300 (n=8), SPEN (n=7), and ADAMTSL3 (n=7), which were all mutated in both groups. The genes associated with the non-canonical NFκB pathway were found to be more frequently mutated in the DAT+ group, with 6 mutations in the DAT+ group compared with 1 mutation found in the DAT- group. Within the DAT+ group, three mutations were found in BIRC3, a gene involved in apoptosis regulation and previously linked to type 1 diabetes mellitus.
There was a non-significant difference in overall survival between the DAT+ and DAT- groups (p=0.19), with a trend towards DAT+ patients being less likely to survive. DAT significantly influenced the effect of R-IPI on survival (p=0.017). Within the DAT- group, R-IPI maintained its strong predictive power for overall survival with three clear groups (p <0.0001). Within the DAT+ group, no patients fell into the "very good" R-IPI prognosis group, while the other two R-IPI groups were not significantly different in their overall survival (p=0.74).
Conclusion
Both DAT positive and DAT negative patient groups showed high rates of non-synonymous mutations in genes that are frequently targeted in DLBCL. These findings suggest mutations in the non-canonical NFκB pathway, which is associated with lymphomagenesis and autoimmunity, may be more common in patients who are DAT positive. This study did not demonstrate a significant effect on survival of DAT positivity in patients with DLBCL, but a moderating influence on R-IPI's survival effect. This moderation may indicate that autoimmunity negates the survival benefits of a better patient risk profile.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal